Emerging
Strategies for the Treatment of Systemic Sclerosis.
Journal
of Scleroderma and Related Disorders.
Volume
1 Number 2 May - August 2016.

Emerging
Strategies for the Treatment of Systemic Sclerosis.
Journal
of Scleroderma and Related Disorders.
Volume
1 Number 2 May - August 2016.
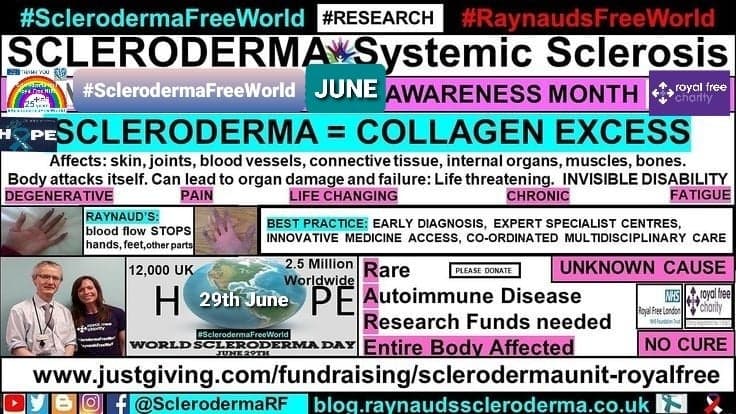
Living with a chronic, progressive, degenerative disease, to which there
is currently no cure, makes you discover inner strength which you did not know
you had.
As Bob Marley sang ‘You do not know how strong you are, until you have
to be’.

Not only does a
scleroderma diagnosis bring along a multitude of debilitating life hijacking
symptoms, this is combined with the current reality that there is no cure
available or known.
Pharmaceutical
agents used for treating scleroderma target symptom suppression as opposed to
treating or acting on the underlying cause.
Which, also,
currently remains a mystery on the scleroderma, systemic sclerosis pathway.
RESEARCH
I wrote about the
importance of research and its role for the scleroderma patient and the rare
disease patient, Click here
In essence, in my
view, an investment in global medical
research is essential for the scleroderma patient.
The time it takes
for newer biologic innovative medicines to reach the market place needs to
be reduced.
As does, the time
taken to access innovative medicines shown to have an improvement in disease
progression and severity.
Time is a luxury for
the scleroderma patient and for all rare disease patients. Medical research is
making improvements, but patients are quite literally “dying for a cure.”
I am grateful that I
am still around to be a scleroderma patient in the hope that investment and
commitment to accelerate medical research, will instigate a light bulb moment
needed for a ‘scleroderma free world’.
TREATMENTS
During Scleroderma
Awareness month June 2016, the UK published national guidelines for the
treatment and management of scleroderma. Click here
The paper ‘Emerging
strategies for treatment of Systemic Sclerosis’ was published within Volume 1
Number 2 May – August 2016, of the Journal of Scleroderma and Related
Disorders (JSRD)
The authors, Dr
Dinesh Khanna, Dr Jorg Distler, Dr Peter Sandner and Dr Oliver Distler discuss
the current medical understanding of the scleroderma disease process along with
possible biologic pathways responsive to newer drug compounds and their mode of
action.
Here is my brief
synopsis, citing excerpts from the paper, ‘Emerging strategies for treatment of
Systemic Sclerosis’:
‘Introduction
Pathological
features of SSc include microvascular damage, dysregulation of adaptive and
innate immunity, and fibrosis that can involve the skin, heart, lungs, kidneys,
gastrointestinal tract and other organs.
The rate of
progression and extent of organ fibrosis are the primary determinants of
clinical outcome…..
Currently, there are
no treatments that modify the underlying cause(s) of SSc, in part because those
causes are incompletely understood.
Thus, current
therapies generally target disease complications, including organ involvement.
Early diagnosis of
SSc, and assessment and treatment of organ involvement, are critical aspects of
patient management because organ involvement is responsible for most of the
complications and mortality in SSc…..
Furthermore, efforts
to identify and validate circulating biomarkers to assess rate of progression
and organ involvement are evolving rapidly.’
The Paper estimates
a prevalence of 300-500 cases per million adults in the US, with another
population-based sample in Canada consistent with his estimate, 443 cases per
million.
This is thought to
vary in the EU, 31-88cases per million in England, to 158, 154, and 277 cases
per million in France, Greece and Spain respectively.
Higher incidence in
women than men (ratios of 4.6 to 5.7:1).
There is also
evidence for difference in prevalence across racial and ethnic groups, with
rates slightly higher among blacks than whites, lower among people of Asian
ancestry, and higher in some Native American groups.
Severity of disease
and its course can also vary according to gender and ethnic background.
For example, black
patients are more likely than white patients to have diffuse cutaneous disease,
and black patients have a higher risk of mortality.
Even though the
prevalence of SSc is lower in men than women, on average male patients with SSc
have a worse prognosis and higher disease-specific mortality than female
patients.
Emerging
Treatment Strategies
'Identification of
several key pathways in the SSc process have opened potential targets for
therapies.
These pathways
include vascular damage and immune activation, and, the fibrotic pathway.
The vascular damage
can be seen by reductions in the number of capillaries and narrowing of the
vessel lumen leading to impaired blood flow and starving the tissues of oxygen.
This produces
inflammation and overactivation of immune cells, with less inflammation in
later disease but persistent activation of the immune system.
RITUXIMAB acts on reducing the excessive circulating immune B cells.
A recent study
reported that it had significantly reduced the modified mRSS compared with
matched controls, these patients also showed a less decline in lung function.
Ongoing trials are
exploring the efficacy and safety of rituximab in SSc associated polyarthritis
(NCT01748084) and SSc-associated PAH (NCT01086540).
These trials will
also provide information about anti-vasculopathic, anti-fibrotic, and immune
modulatory effects of rituximab.
ABATACEPT acts on immune T cells deactivation.
A small study in
patients with SSc-related refractory polyarthritis or myopathy found that
abatacept significantly improved joint parameters, although there was no change
in skin or lung fibrosis.
However in another study,
abatacept was shown to have significant improvement on Mrss score.
These results
suggest that it may be possible to identify a subset of dcSSc patients most
likely to respond to abatacept.
A phase II
multicenter international trial is underway to study abatacept in patients with
dcSSc; the trial uses skin fibrosis as the primary endpoint (NCT02161406).
Fibrosis
Evolving
understanding of the SSc disease process indicates that vascular and immune activation
initiate a fibrotic process that then becomes self-sustaining through several
mechanisms.
Fibrosis may
continue long after evidence of immune activity subsides in affected tissues.
Thus, many of the
current efforts for developing therapies are focused on interfering with
mechanism responsible for unregulated self-sustaining fibrosis.
Early studies have
shown that skin fibroblasts isolated from patients with SSc continued to
produce higher amounts of collagen and other extracellular matrix components
compared to those fibroblasts from normal subjects.
TRANSFORMING GROWTH FACTOR β (TGFβ)
(TGFβ) has been
recognised as a central mediator of fibrotic signalling in SSc.
This makes it a
natural target for potential antifibrotic therapies in SSc.
The human antibody
metelimumab showed no evidence of a treatment effect, however, fresolimumab has
shown a statistically significant decline in mRSs scores within a few weeks
after administration of one or two doses.
A decline in the
expression of the (TGFβ)-regulated genes thrombospondin-1 and cartilage
oligomeric protein, as well as significant declines in the infiltration of
myofibroblasts into the dermis.
This study was too
small to effectively evaluate adverse effects, although several patients had
bleeding episodes, and anaemia was common.
Soluble guanylate
cyclase inhibitors such as Riociguat and BAY41-2272 are showing promising
results with inhibiting skin fibrosis.
Riociguat is currently
licensed for Pulmonary Arterial Hypertension with an ongoing phase II
multicenter international trial of patients with dcSSc (NCT02283762) underway.
Interleukin-6 (IL-6)
is produced by B cells, T cells, and fibroblasts, and it promotes inflammation
and fibrosis.
Serum IL-6 levels
are elevated in certain patients with SSc, particularly early dcSSc, and these
levels have been suggested to correlate with progression of skin involvement,
worsening lung fibrosis, and reduced long term survival.
However, where
fibrosis is less inflammation dependent, an anti-IL-6 antibody was ineffective.
This finding may
indicate that strategies targeting IL-6 may be most effective in patients with
inflammatory SSc.
Tocilizumab is an antibody to
the IL-6 receptor approved for the treatment of rheumatoid arthritis.
Treatment with
tocilizumab showed significant improvement in joint parameters as well as
improved outcomes with lung resolution.
No statistically
significant change was seen in skin score. A phase III trial of tocilizumab in
SSc is currently recruiting participants (NCT02453256).
Tyrosine kinase signalling pathways
In addition to
(TGFβ), various other growth factors and cytokines are thought to be involved
in promoting fibrosis on SSc, such as connective tissue growth factor (CTGF)
and the platelet-derived growth factors (PDGFs).
Imatinib is a
tyrosine kinase inhibitor (TKI) targeting PDGF, c-abl, c-kit, and has been
shown to prevent fibrogenesis in the laboratory.
So far, the study
results show Imatinib to trend toward increased lung capacity and improved skin
score, making it a possible benefit in the SSc-ILD population at low doses due
to its adverse event profile increasing with dose concentration.
Nilotinib is a TKI active
against the PDGF receptor as well as c-Abl and other tyrosine kinases.
In a small study,
skin scores were improved, as well as predictive markers of response were
evidenced.
Higher baseline
levels of expression of genes related to (TGFβ) or PDGF signalling were
associated with response and expression of these genes declined during
treatment.
Nilotinib was
associated with abnormalities in liver function tests and QTc prolongation, the
latter of which required discontinuation of treatment in two patients.
Dasatinib is another multi
target TKI approved to treat chronic myelogenous leukemia, however, it showed a
high serious adverse event profile in a small scleroderma patient study.
Nintedanib is a TKI-targeting
fibroblast growth factor (FGF) receptor, PDGF receptor, and vascular
endothelial growth factor (VEGF) receptor, as well as Src-family tyrosine kinases.
So far, studies are
showing promising results with skin and lung fibrosis reduction.
A phase III trial of
nintedanib with patients with SSc and ILD is ongoing (NCT02597933).
Pirfenidone is an anti-fibrotic
agent with anti-inflammatory properties including inhibition of
pro-inflammatory cytokines and inhibition of inflammatory cell proliferation. a
controlled clinical trial in patients with SSc-ILD is planned, further to a
safety and tolerability trial results showing dosing tolerability.
The peroxisome proliferator-activated
receptor-γ (PPAR-γ) is a key suppressor of fibrosis.
A genome-wide
association study provided evidence for a role of PPAR-γ in susceptibility to
SSc and PPAR-γ is downregulated in patients with SSc.
However, caution is
exercised as the use of PPAR-γ agonists increases cardiovascular event risk.
So far, the drug
molecule IVA337 has not been associated with this adverse event and is the
subject of an ongoing proof-of-concept phase II trial in patients with dcSSc
(NCT02503644).
Lysophosphatidic acid (LPA) related ligands
Mouse models have
shown that by blocking this receptor, fibrosis is reduced. Studies have shown
the chemical compound SAR 100842 to reduce expression of fibrosis related genes
in SSc skin fibroblasts, with patients treated with SAR100842 showing a decline
in skin score.
CONCLUSION
Management of SSc
still rests on the treatment of organ specific complications, and no
disease-modifying therapies are yet available.
However, recent
years have seen major advances in our understanding of the pathophysiologic
processes responsible for the immunologic fibrotic mechanisms of disease.
This is complemented
by development of better outcome measures and data driven approaches to assess
for cohort enrichment.
Concurrently,
studies in large patient cohorts have yielded valuable insights into clinical
and laboratory markers of disease activity and prognostic markers of
progression, which should serve to identify clinically relevant disease
subtypes to refine enrolment criteria for clinical trials.
Considered together,
these advances hold great promise for the development of disease modifying
therapies that will improve the well-being of patients with SSc, reduce or
prevent complications of the disease and ultimately prolong survival.’
In the meantime, I
know that I am fortunate to now be 13 years immunosuppressant and chemotherapy
free.
I will continue to
“Live the dream, Scleroderma Style,” with hope, remaining as my best
friend and companion – I even have the T-shirt.
To read JSRD Volume 1 Number 1 Jan – April 2016, Click here



April 2017.
To read my articles:

Rare Disease Day 2018, Research - Taking Part in Clinical Trials, Click here
March Autoimmune Disease Awareness Month 2018, Click here
Global patient video, Click here
Becoming a Patient Research Ambassador for the NIHR, Click here
If we only had more RESEARCH investment for Scleroderma, Raynaud's, Autoimmune Rare Disease, Click here
The Importance of Medical Research and Awareness to the Scleroderma, Raynaud's, Autoimmune Rare Disease patient, Click here

The Pandora’s Box of the rare autoimmune disease
Scleroderma, Raynaud's and Cancer, Click here


World Scleroderma Day 29th June 2017, Click here
Why Global Collaboration is important to the Rare Disease Patient, Click here

RARE DISEASE DAY:
Rare Disease Day 2018 – Research, Taking
Part in Clinical Trials. Scleroderma, Raynaud's, Autoimmune Rare Disease, Click here
2016 Rare Disease Day Patient Voice
2016 Rare Disease Day Patient Voice


Rare
Disease Day is a fantastic opportunity for the entire rare disease
community to shine a spotlight on their reality, combining as one unified
voice. Where, at least one commonality presides –
Medical
Research provides the brightest light
for the illumination of the rare disease
patients’ plight.
I
highlighted other areas of medical research interest within Week 3 of my Patient Profiles Campaign for Scleroderma Awareness Month 2017.
VIDEO
VIDEO

Although
rare disease patients are few in number, eg. 2.5 million scleroderma patients
worldwide, (the World Scleroderma Foundation), the commonalities and golden
hallmark for each rare disease patient are the same:
Early Diagnosis
Expert Specialist Centres
Access to Innovative Medicines
Where MEDICAL RESEARCH investment
is VITAL.
Research
is the key. Abstracts from 2016 World Congress, Click here


The Family Day at the Scleroderma Unit, The Royal
Free Hospital is taking place on the 19th May 2018. Browse the
program, here
This year, I am celebrating 20 years of being a
patient at this world leading expert specialist research centre.
 |
| Sept 2017 |
I am eternally grateful to the global scleroderma
trail blazers Dame Prof Black and Prof Chris Denton, whose commitment and
dedication to unlocking the scleroderma enigma, is nothing other than,
superhuman.
I am truly humbled and inspired by their work
ethic. I am wholly appreciative for Prof Denton’s continued medical expertise
and support, especially during my barrister qualifying years, 1997 -
2004.
1st March 2004, I qualified as a self
employed practising barrister. Further to having been told in 1997, by my
diagnosing doctor, that I was looking at a 15month prognosis.
I very much hope to utilise my professional skills
and qualifications along with my patient experience, to help achieve the
#SclerodermaFreeWorld dream, hoping to improve understanding and best practice,
in the meantime.
For latest updates follow:

Facebook Page:
Twitter: @SclerodermaRF @RaynaudsRf
Google Plus: Raynauds Scleroderma Awareness Global Patients
#SclerodermaFreeWorld
#RaynaudsFreeWorld
#ADAM #Scleroderma
#Raynauds
#RareDisease
Living the dream, scleroderma style.

Please DONATE to help
fund medical research at The Scleroderma Unit,The Royal Free Hospital, London.

100% of your monies will be used for medical
research purposes only. No wages or admin costs. Thank You.
#HOPE



Last Update: April 2018